Menopause And Polycystic Ovary Syndrome
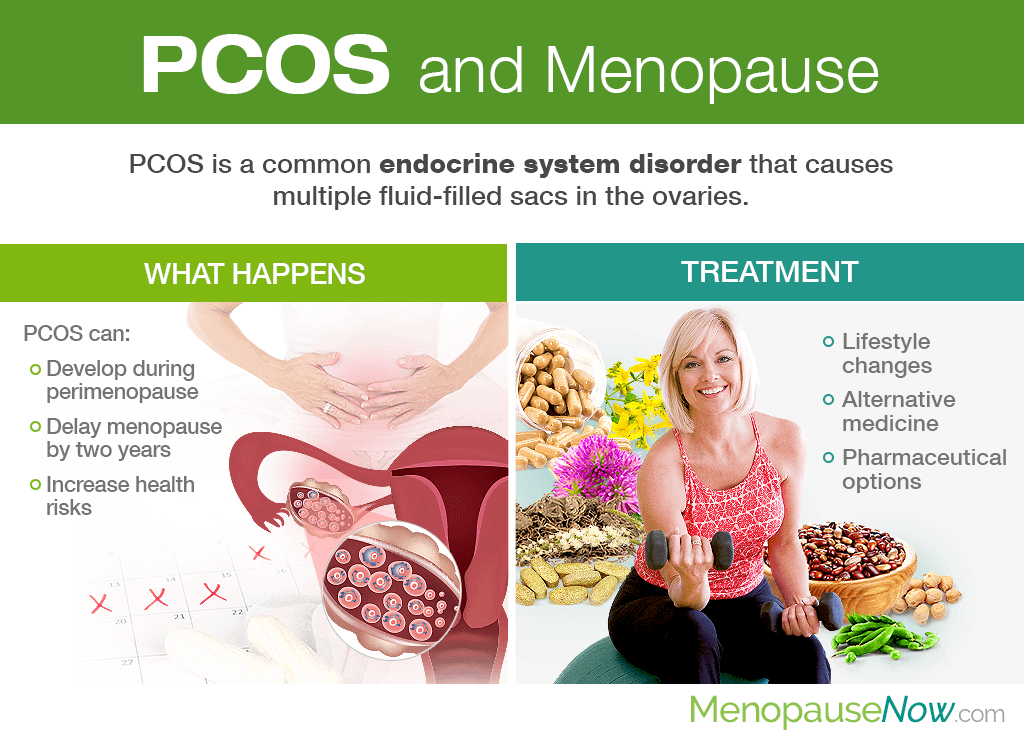
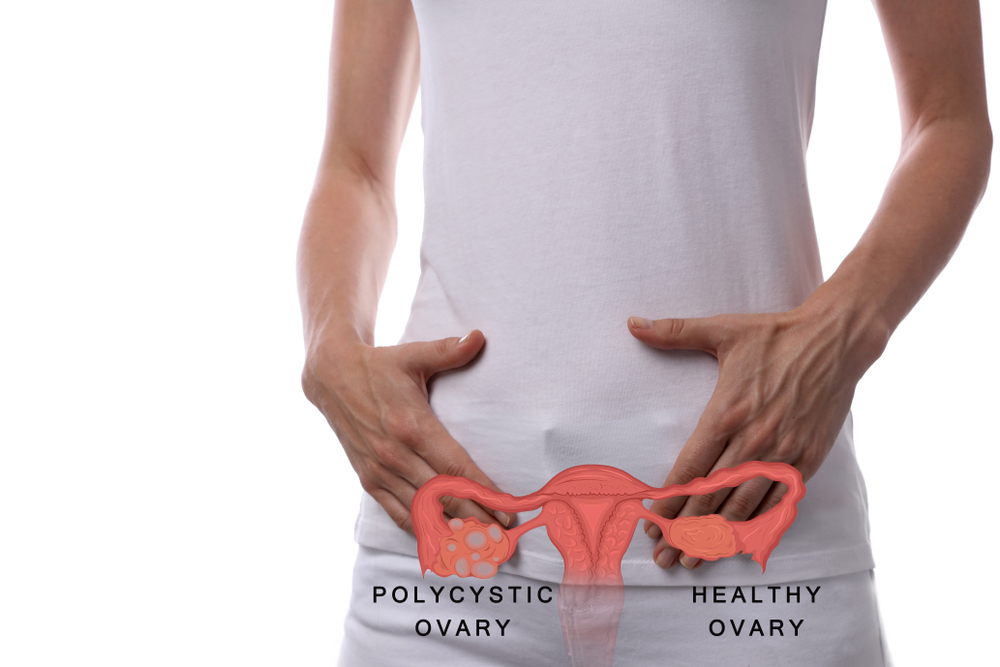
Menopause and polycystic ovary syndrome. Find out what happens to PCOS when hormones change at menopause. Polycystic ovary syndrome PCOS is a condition that leads to cysts growing on a womans ovaries. Polycystic ovary syndrome PCOS has been extensively studied in reproductive-aged women.
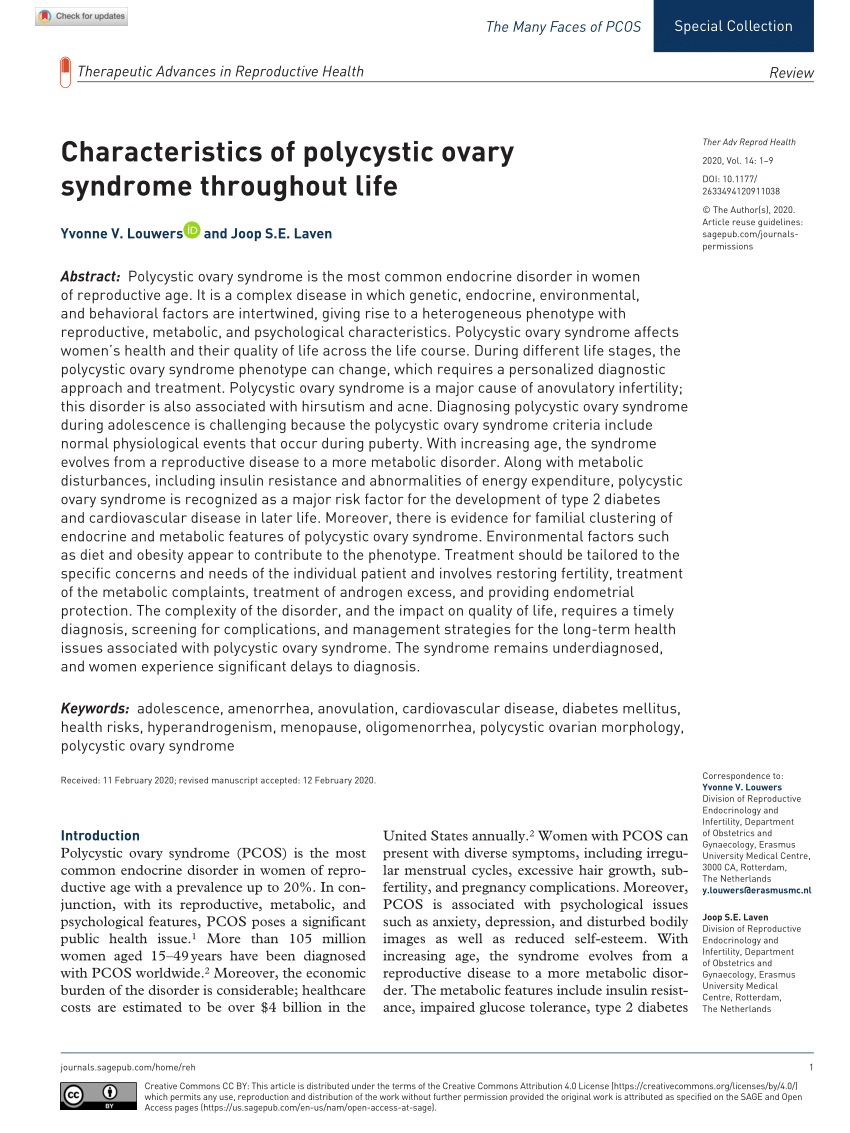
Moreover PCOS may increase a womans risk for. The evidence indicates that PCOS is associated with long-term health risks including type 2 diabetes metabolic syndrome obstructive sleep apnea endometrial cancer and mood disorders. PCOS can affect the onset and course of menopause and cardiovascular health in perimenopausal and postmenopausal patients.
While testosterone levels can rise a bit after menopause they can be elevated due to PCO or due to other conditions that need to be ruled out by consultation with a physician. Menopause is when a. These evidence-based tools have been informed by the latest research and clinical expertise.
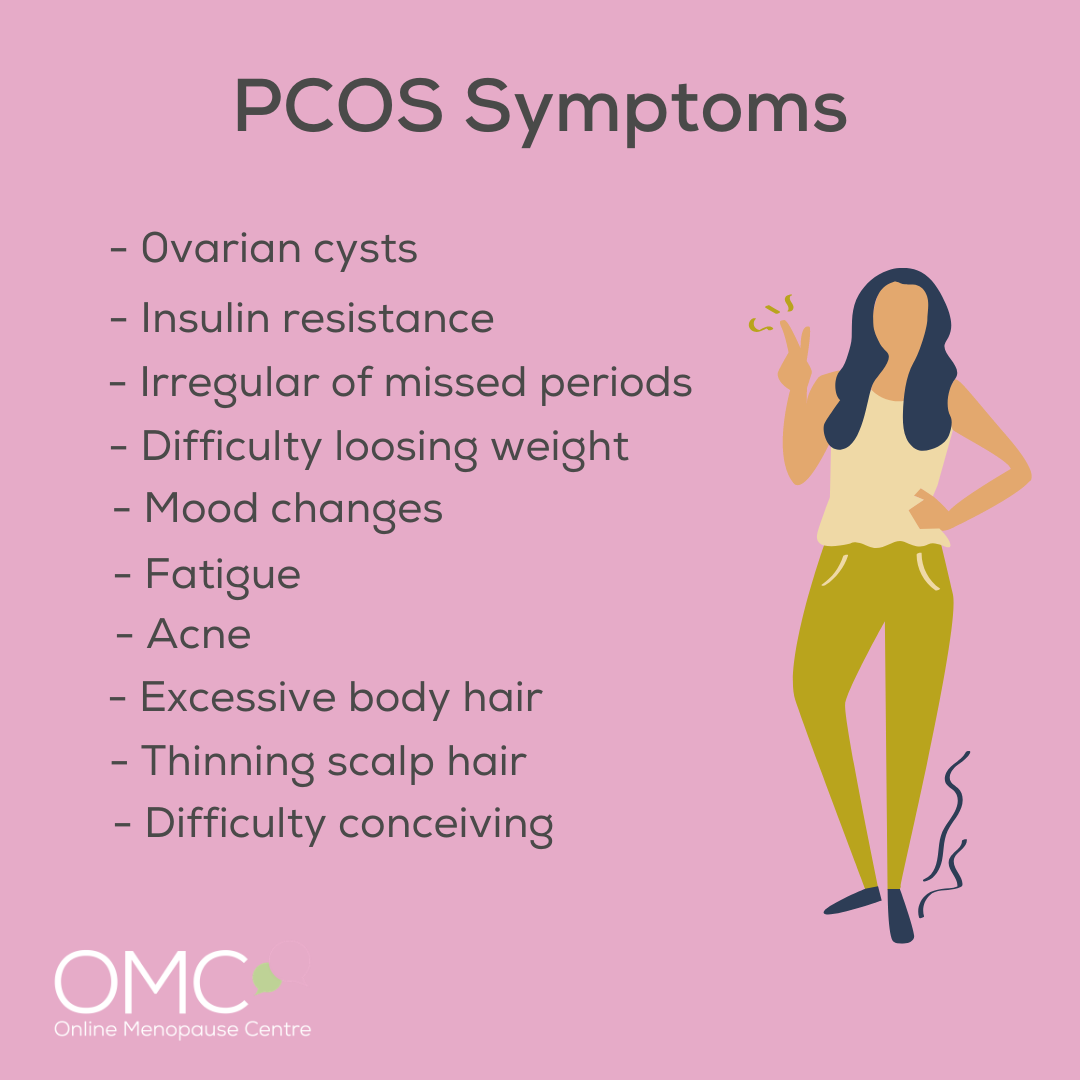
Hot flashes and negative changes in cholesterol panels are symptoms of menopause. In these pages you will learn all about the causes signs and symptoms of PCOS how it is diagnosed and what treatments are available to help. 1 irregular menstrual cycles or anovulation 2 hyperandrogenism and 3 PCO morphology.
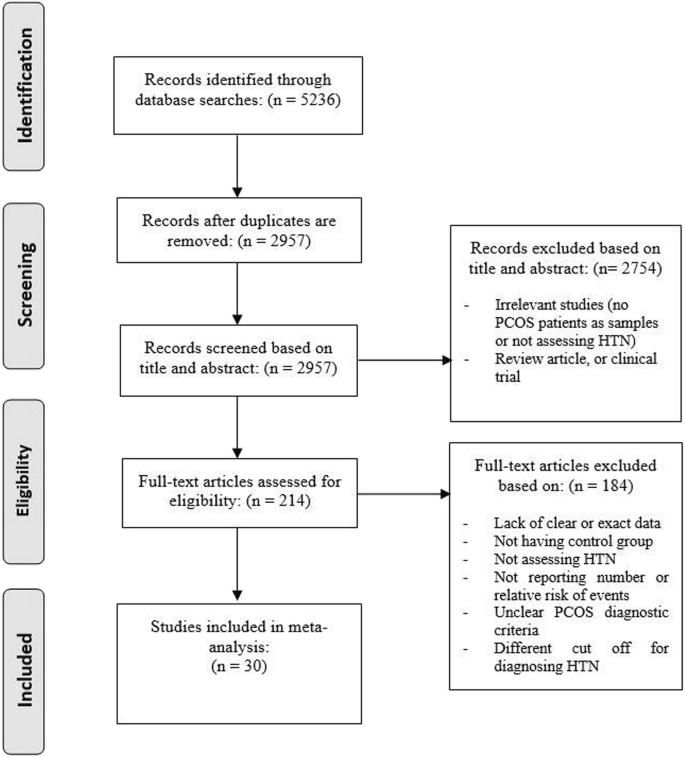
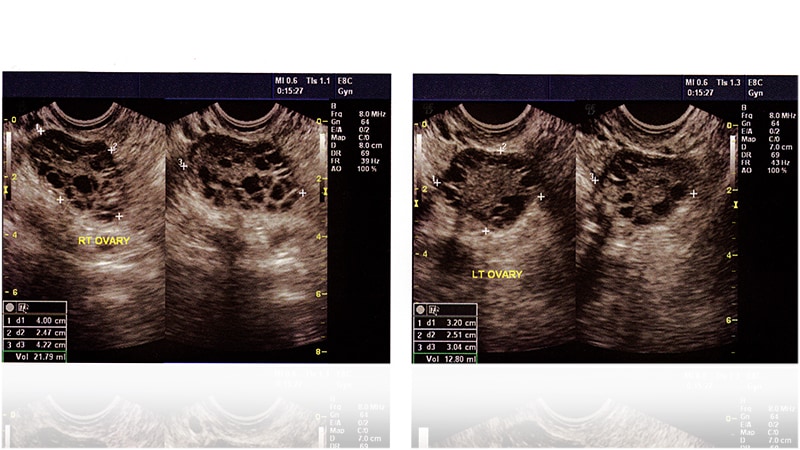
PCOS can be diagnosed by taking a medical history examination blood tests and an ultrasound. PCOS can be associated with problems such as irregular menstrual cycles excessive facial and body hair growth acne obesity reduced fertility and increased risk of diabetes. PCOS Polycystic ovary syndrome PCOS is a common health condition that affects 8-13 of women of reproductive age.
GOOD news for women with polycystic ovary syndrome not normally a cause for celebration. T2 - Polycystic Ovarian Syndrome Menopause and Osteoporosis. Polycystic ovary syndrome PCOS is diagnosed during the reproductive years when women present with 2 of 3 of the following criteria.
It is more common in some high-risk groups such as Indigenous women. A total of 545 of women report use of at least one CIM approach specifically for.
AU - Ring Melinda.
It happens when the sex hormones progesterone and estrogen are out of balance. Not only are they just as likely to have children as any other woman but they have a better chance of. Women suffering from polycystic ovary syndrome experience irregular menstrual cycles imbalanced hormones and an increased risk of infertility. PCOS can affect the onset and course of menopause and cardiovascular health in perimenopausal and postmenopausal patients. PCOS can be associated with problems such as irregular menstrual cycles excessive facial and body hair growth acne obesity reduced fertility and increased risk of diabetes. Menopause is when a. Jean Hailes for Womens Health has developed practice support tools for health professionals for the assessment and management of endometriosis heavy menstrual bleeding menopause and polycystic ovary syndrome PCOS. The methods used by doctors to address the symptoms of women with PCOS while in menopause take into consideration the issue of higher androgens when developing a protocol. These evidence-based tools have been informed by the latest research and clinical expertise.
Polycystic ovary syndrome PCOS has been extensively studied in reproductive-aged women. 1 irregular menstrual cycles or anovulation 2 hyperandrogenism and 3 PCO morphology. Polycystic ovary syndrome PCOS is a common endocrine disorder involving an imbalance of reproductive hormones that affects up to 10 percent of women of reproductive age. PCOS can be associated with problems such as irregular menstrual cycles excessive facial and body hair growth acne obesity reduced fertility and increased risk of diabetes. PCOS Polycystic ovary syndrome PCOS is a common health condition that affects 8-13 of women of reproductive age. Menopause is when a. However accumulating research shows that PCOS can have lifelong effects on multiple aspects of womens health.





































Posting Komentar untuk "Menopause And Polycystic Ovary Syndrome"